
Connexus PCN Pharmacy Team
The PCN Pharmacy team is a team of pharmacists, pharmacy technicians and prescription clerks working across all 5 surgeries. Our pharmacists are trained healthcare professionals, specialising in medicines.
The pharmacy team help patients to manage their prescriptions, they advise on medications and deal with any queries, and ensure that prescribed medications are reviewed and safe for patients.
Our practice pharmacists help manage long-term conditions, such as hypertension and diabetes, to ensure that the medication patients have been prescribed is working and is the right medication for them.
What do we offer?
The team’s role is to help provide focused medication reviews looking to help patients who are on large numbers of medications or medications that carry risks.
The team is here to help inform you why you are taking the medications and what their role is in your long-term care, how to use the medications in a way that you can get the maximum benefit from them and provide you with practical tips on managing your conditions and medication routines.
The goal of the pharmacy team is to help ensure that patients are not only taking their medications but making sure that they are taking only what is necessary. They ensure that medication is being used in the right ways and provide you with support in managing your medications and conditions.
How to access this service
Your GP Practice have a dedicated team of care coordinators who can help signpost you to the right services for your needs.
Repeat Prescriptions
Always check how many days of medication you have left before ordering more and keep track of what you have left so you don’t run out.
We advise that you only order more medication when you have about 7 days’ worth left. Before requesting your medication, check your cupboards first and ONLY order what you need.
Please allow at least 5 working days before collecting your medication from your pharmacy if sent electronically; this is to allow time for any necessary checks to be done by the prescriber before the prescription is signed off and to allow the pharmacy team to process the prescription, order, dispense and check the medication. Ordering specials may take longer. Paper prescriptions can be collected from the surgery in 3 working days.
Ordering your repeat prescriptions:
You can order your repeats in a number of ways.
Email – you can email your request to bnssg.connexus.prescribing@nhs.net
All emails must include your name, date of birth and the surgery you are registered at.
Via App –
These are the 2 preferred apps to use (Please check with your surgery which one is used by them) – you can then choose to use your computer or smart phone and the prescription request is delivered straight to our clinical system:
NHS App and your NHS account – NHS (www.nhs.uk)
The NHS App can also be used to access your Covid pass as well as ordering your repeat medication. It is also possible for family members and carers to order repeat prescriptions on someone’s behalf through ‘linked profiles’ which is useful for those who are housebound or frail.
Patient Access – GP appointments & prescriptions online
Patients can also submit an E-consult with their queries.
In person – you can order via your chemist.
See useful resources below:
How to get started on Patient Access
Patient Access introduction – GP services at your fingertips – YouTube
Connexus PCN First Contact Physiotherapy Team
First Contact Physiotherapists (FCP) are expert musculoskeletal (MSK) clinicians We have introduced this role to reduce the workload on GPs and ensure your wait for an appointment is reduced.
Lower back and neck pain are the greatest cause of years lost to disability in the UK, with chronic joint pain or osteoarthritis affecting more than 8.75 million people. In addition, musculoskeletal conditions also account for 30% of all GP appointments. By 2024, all adults in England can see a musculoskeletal first contact physiotherapist at their local GP practice without being referred by a GP.
What does a First Contact Physiotherapist do?
They are specialists in assessment of musculoskeletal (MSK) issues and have the same ability as GPs to refer patients for further investigations, local community physiotherapy or further specialist assessment in secondary (next level) services such as the musculoskeletal interface (MSKI) service or other hospital-based specialists if required.
They will assess and diagnose patients with MSK issues, guide on initial management and refer on for additional care if required. This may include:
- advice on a home exercise plan
- steroid joint injections
- requests for medication prescriptions
- referral for further investigations (e.g., X-Ray, Blood tests)
- referral for community physiotherapy
- referral to orthopaedics (e.g., MSK CATS)
- referral for other services (e.g., social prescribers)
The benefits
By making it easier for patients to access specialist assessment in the practice, patients may have quicker access to diagnosis and treatment. This will help them manage their conditions more effectively and recover well, supporting a prompt return to everyday life. FCP physiotherapists help GPs to manage their workload more effectively and reduce the need for onward referrals.
How to access this service
You can self-refer or may be referred by your GP, nurse or health visitor.
Our FCP physiotherapy team are unable to provide on-going rehab themselves in the practice and work differently to traditional or ‘in-house’ physiotherapists.
Connexus PCN Paramedic Team
Paramedics work autonomously within the community using their enhanced clinical assessment and treatment skills, to provide first point of contact for patients presenting with undifferentiated, undiagnosed problems relating to minor illness or injury, abdominal pains, chest pains and headaches. They are health professionals who have the capability to make sound judgements in the absence of full information and to manage varying degrees of risk when there are complex, competing or ambiguous information or uncertainty.
What does a Paramedic do?
- Assesses and triages patients, including same day triage, and as appropriate provide definitive treatment or make necessary referrals to other members of the PCN team.
- Advises patients on general healthcare and promote self-management where appropriate, including signposting patients to other community or voluntary services.
- Carries out:
a. specialist health checks and reviews.
b. ECGs; alongside other results as appropriate.
c. investigatory procedures as required.
d. undertakes the collection of pathological specimens including intravenous blood samples, swabs, etc.
e. investigatory procedures needed by patients and those requested by GPs and the wider PCN. - Assesses and review patients as required by our care homes via planned booked appointment lists, liaising with nursing teams in the homes, formulating management plans and delivering high standard care and support to the homes.
- Support the delivery of anticipatory care plans and lead certain community services (e.g., monitoring blood pressure and diabetes risk of elderly patients living in sheltered housing).
- Collaborates with other members of the PCN including doctors, nurses and other AHPs, accepting referrals and referring to them for specialist care.
- Clinically examine and assess patient needs from a physiological and psychological perspective and plan clinical care accordingly.
- Prioritises health problems and intervene appropriately to assist the patient in complex, urgent or emergency situations, including initiation of effective emergency care.
- Diagnoses and manage both acute and chronic conditions, integrating both drug- and non-drug-based treatment methods into a management plan.
- Supports patients to adopt health promotion strategies that promote healthy lifestyles and apply principles of self-care.
How to access this service
You can be referred by your GP or an Advanced Nurse Practitioner (ANP).
Connexus PCN Social Prescribing Team
Social prescribing is a way GPs, nurses, link workers and other health and care professionals can refer people to a range of local services to meet their non-clinical needs.
Recognising that people’s health is determined primarily by a range of social, economic and environmental factors, social prescribing seeks to address people’s needs holistically. It also aims to support individuals to take greater control of their health.
Social prescribing schemes can involve various activities typically provided by voluntary and community sector organisations. Examples include volunteering, art activities, group learning, gardening, befriending, cooking, healthy eating advice and various sports.
Who is it for?
It is a free service whereby Social Prescribing Link Workers support you in accessing in a range of local services, organisations and activities. The main aim is to help improve your overall health and wellbeing. If you are feeling isolated, struggling to get out and about, need practical support or want to focus on your mental wellbeing, we can help.
What are the benefits?
Some of the benefits of social prescribing include:
- Support at the right time.
- Space to consider options and be listened to.
- Increased feeling of connectivity with their community.
- Increased confidence.
- Improved mental health.
- Increased physical activity levels.
- Reduced feelings of loneliness and isolation.
- Improved health and wellbeing.
- Improved levels of self-management of long-term conditions and increased resilience.
How to access this service
You can refer yourself to the service by speaking to a member of your GP practice team. You do not need an appointment to do this, you can just drop in and ask at the front desk or you can be referred by the person you are seeing within your GP practice if you have an appointment.
Connexus PCN Mental Health Team
The Connexus PCN Mental Health team comprises of one full time Mental Health Practitioner (MHP) (seconded from AWP) and three Mental Health and Wellbeing Coaches (MHWC). The role of the team is to support patients who present with mental and emotional health needs which would benefit from longer initial consultation and if appropriate follow up appointments.
Who is it for?
The service is for patients aged 18 and over only. The service can see people who are on a waiting list for another service, but not if they are having or just about to begin active treatment (i.e AWP, VitaMinds, private therapy/counselling).
What do we offer?
We support people who are suffering from a wide range of mental health conditions, including people with high levels of need and complexity. We have introduced Mental Health Practitioners to support individuals in the community. Our Mental Health Practitioner will see patients with more severe health presentations or existing diagnosis. We offer pre booked and same day 20-minute appointments.
Our mental health team also consists of Mental Health and Wellbeing Coaches (MHWC). The role of the Mental Health and Wellbeing coaches is to see patients who have mental and emotional health needs which do not meet the threshold for the Mental Health Practitioner. This includes support for people struggling with panic/anxiety, low self-esteem, bereavement/loss/grief impacting on their mood, depression/low mood, sleep hygiene and chronic pain. We offer a 40-minute appointment for our new patients for initial assessment and agreement of a personalised care plan to address the patient’s emotional health and wellbeing needs. Patients will be offered up to five follow up appointments depending on their needs.
*NB: It should be noted that neither the Coaches or Practitioners are Counsellors and therefore do not offer a counselling service.
The benefits
By making it easier for patients to access mental health support, patients will have quicker access to diagnosis and treatment. This will help them manage their conditions more effectively and recover faster, so they can return to normal life quickly. It will also help GPs to manage their workload more effectively and reduce the need for onward referrals.
How to access this service
You can access this via your GP practice, or you can self-refer.
To self-refer to this service, please email bnssg.connexus.pcn@nhs.net and list your name, date of birth, and GP surgery.
Pain Clinic
If you have had pain for more than 3 months, that has not resolved you may be interested in this clinic.
If all investigations are complete, and no further intervention is planned, but you remain in persistent pain, this clinic may be for you!
A Physiotherapist, Pharmacist and Social Prescriber run this one-off session to hear your experience with pain, how it is affecting you, and work with you to form a pathway forwards.
Persistent pain can eat away at so many aspects of your life. This clinic can help you navigate your way back to living, even if the pain remains unresolved.
This is a one stop clinic available through referral from your clinician or you can self-refer by emailing bnssg.connexus.pcn@nhs.net with your name, DOB, and which surgery you are registered with.
The clinics are currently held bi-monthly at varied locations across the PCN.
Joint Injection Clinic
Steroid Injection

Why have I been prescribed a steroid injection?
Steroid injections are used to reduce inflammation in joints or areas of pain. They can be used as part of the treatment for joint pain and soft tissue problems. Your doctor, nurse or physiotherapist has made an assessment of your condition and feels that a steroid injection may offer you some symptom relief and help your pain.
What does a steroid injection contain?
There are different types of steroids that can be injected. We normally use the steroid ‘Depo-medrone’ for joint injections and combine this with a local anaesthetic called ‘Lidocaine’. Together the steroid and local anaesthetic can effectively reduce inflammation and pain allowing you to feel more comfortable and function more easily.
How long does the steroid injection take to work?
You should start to notice an improvement in your pain after one week. Some patients have a beneficial effect prior to this.
Do I need to take any precautions after my steroid injection?
You should rest for 1-2 days after your steroid injection. During this time you should use the joint as you normally would but avoid heavy lifting or strenuous exercise of the area that has been treated. You can take your regular pain killing medications such as paracetamol. If you already have a physiotherapy exercise programme in place for your condition it is normally fine to continue this soon after your injection and the effects of the injection will often make your physiotherapy exercises easier to do.
Can I leave the surgery after my steroid injection?
As with all medications there is a small risk of an allergic reaction to the contents of the steroid or local anaesthetic. Allergic reactions can still occur even if you have had the steroid injection previously. It is advised that you sit in the waiting room for 15 minutes after your injection. If you feel unwell in this period please inform a member of staff.
What are the risks or side effects of having a steroid injection?
Side effects from the injection are rare. Occasionally people notice a flare in their joint pain in the first 24-48 hours of having a steroid injection. This normally settles down within a couple of days and then the pain should start to improve.
A very rare side effect of a steroid injection is infection in the joint or tissue. For every 20,000 patients given an injection only one patient is likely to suffer from an infection following a joint injection. If your joint becomes more and more painful, is red, swollen and hot, or if you develop a temperature then you should seek medical help. Do not wait for this to settle down.
Occasionally a blood vessel can be ruptured after having a joint injection.
Steroid injections may cause facial flushing and interfere with your periods.
Steroid injections may cause a change in your mood. This is unusual but you are more at risk if you suffered with mood disturbance before your injection. Please discuss this with your GP if you are concerned.
People sometimes notice dimpling or pigmentation change over the site where the steroid injection is given.
Another rare side effect to having a steroid injection can be damage to the tendon within the joint. This tends to occur when tendons are already weakened or damaged.
What else should I know about steroid injections?
Repeating a steroid injection to the same joint too many times can have a negative effect on the joint and cause deterioration of the cartilage or soft tissues. The general rule of thumb is to limit the number of repeat injections to a maximum of 3-5 times for a single joint. You should have a discussion with your GP or Physiotherapist about the pros and cons of repeating an injection as the number of repeat injections can depend on what part of the body is being injected.
If you are a diabetic the steroid may increase your blood sugars for a week after the
injection. Your blood sugar should be monitored more closely than normal after an
injection of steroid.
We don’t recommend the use of steroid injections during pregnancy. However steroid injections should not affect your fertility.
If you are on blood thinning medications we may not be happy to inject you with steroid. Your referring GP, nurse or physiotherapist will have discussed this before recommending a steroid injection to you.
Steroid injections may delay healing from a wound or post-surgery. It is therefore not
advisable to receive them during this time of healing.
It is not advisable to have a steroid injection within 2 weeks before a planned COVID-19 vaccination/booster OR sooner than 2 weeks after the vaccination/booster.
It is also not advisable to have a steroid injection until 4 weeks after testing positive for COVID-19. You should have made a good recovery from COVID before having a steroid injection.
References and further information
Arthritis Research UK https://www.versusarthritis.org/about-arthritis/treatments/drugs/steroid-injections/
Patient UK www.patient.co.uk/doctor/joint–injection-and-aspiration
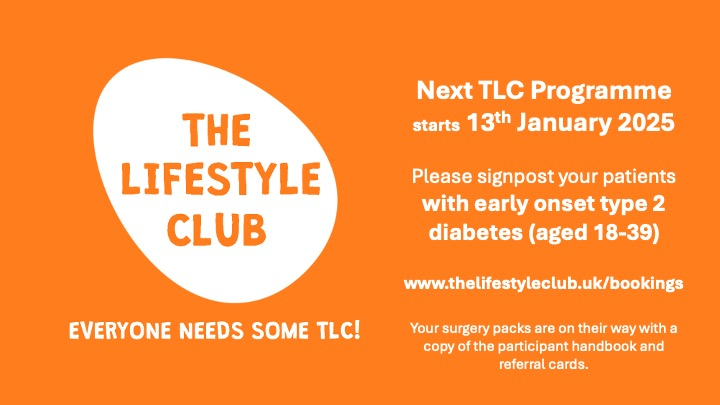
You can register for an Information Session at www.thelifestyleclub.uk/bookings
